Eye and thyroid
Definition
Dysthyroid orbital (OD) or Grave's disease or thyroid eye disease (TED's) in Anglo-Saxon is an autoimmune inflammatory disease linked to the thyroid gland. It affects the periocular orbital structures, muscles, fat, and eyelids.
OD can be associated with various disorders of the thyroid gland, it is frequently observed in patients with hyperthyroidism, but also in patients with hypothyroidism and even in patients without thyroid abnormality.
Thyroid disease can cause multiple eye symptoms that vary from one individual to another depending on its severity = sensation of irritation or foreign bodies, redness, conjunctival edema, diplopia (double vision), loss of vision, eyelid retraction, eye protrusion or exophthalmos, there may also be decreased eye movements, incomplete eye closure rarely corneal ulceration or optic nerve compression, or reduced visual acuity.
Understanding the disease
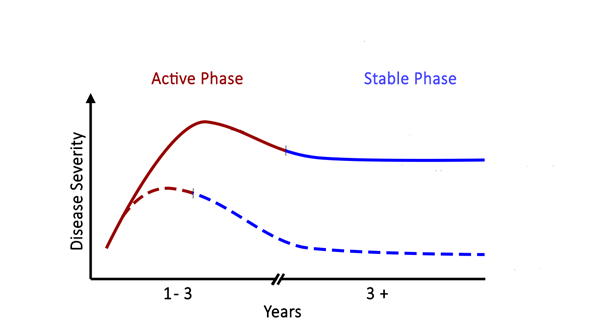
Dysthyroid orbital disease goes through two phases, an active phase and a stable phase, where the disease does not progress. During the active phase there is an immune inflammatory process which will cause the appearance of clinical signs and especially the aggravation of the disease. The goal of treatment is to shorten the active phase of DO over time and to decrease the severity of the disease. (See the curves below)
How to diagnose ?
Dysthyroid orbital (OD) is usually associated with other symptoms of hyperthyroidism, however the clinical symptoms of an overactive thyroid are not always present. OD can occur even before the thyroid imbalance.
The ophthalmologist can diagnose a thyroid imbalance by finding clinical signs in favor of DO.
Computed tomography (CT) or magnetic resonance imaging (MRI) are indicated to assess oculomotor muscles and periocular fat and other signs of inflammation.
OD often improves spontaneously. However, in some patients, symptoms may persist despite treatment for the overactive thyroid gland and OD.
Prevention
In the face of a thyroid imbalance, the presence of signs of dysthyroid orbitopathy (OD) is not systematic, their appearance is unpredictable. OD signs cannot be avoided or prevented.
Treatment of hyperthyroidism with radioactive iodine may make DO worse. Its use is discussed in front of eye signs. It should be avoided, if possible in patients with severe eye damage. Taking a corticosteroid (prednisone) at the time of treatment for several weeks can prevent worsening of DO.
Treatment with antithyroid drugs or thyroid removal surgery does not affect the course of dysthyroid orbitopathy.
The smokers are likely to develop an OD, cause a worsening and a longer duration of the disease than the non-smokers. Passive smoking is as dangerous as active smoking and should be avoided.
Stopping smoking is essential to avoid forms resistant to treatment as well as serious forms.
The treatment
If you suffer from ocular signs of dysthyroid orbital disease, certain actions and treatments may be beneficial and provide relief.
Prevent risk factors for dysthyroid orbital disease
- - the tobacco
Tobacco users have more severe forms than non-tobacco users Tobacco users respond late and less well to medication Stopping smoking reduces the risk of developing diplopia (double vision) or exophthalmos (the eye that moves forward or comes out of its place)
- - Hormonal balance
Restoring hormonal balance with synthetic antithyroid drugs improves DO. Treatment of the thyroid with radioactive iodine may cause the development or deterioration of DO especially in ++++ smokers. Thyroidectomy (removing the thyroid) does not affect the course of DO. The onset of clinical signs of OD may be associated with uncontrolled hypothyroidism.
Eat selenium
It is an antioxidant and anti-inflammatory agent that plays a role in the activity of the thyroid gland and the immune system. It also improves the quality of life and the clinical signs of DO.
Wear sunglasses
The eyes are more vulnerable to ultraviolet rays and more sensitive to the sun. Wearing sunglasses helps protect them from the sun and wind.
Use lubricating eye drops
Artificial tears, can help relieve dryness and tingling. A lubricating gel can be used before bed to protect the cornea against the environment and dryness especially in front of lagophthalmos or inability to completely close the eyelids during sleep.
Elevate the head of your bed
Keeping your head higher than the rest of your body can decrease edema and help relieve eye pressure.
Prisms
In the presence of diplopia (double vision), glasses containing prisms may be prescribed by your doctor. However, in a few cases the prism is out of place and the indication for extra ocular muscle surgery would be more effective.
Medical treatment
Glucocorticoids. (Prednisone)
Plays an important role in the active phase of the disease to improve or stop the progression of the disease.
Intravenous glucocorticoids are 70 to 80% effective.
Oral glucocorticoids have a lower efficacy between 50 and 65%.
Well-conducted treatment regimens can be made to target inflammation and treat DO.
Specific treatments
Are used in case of contraindication or non-response to corticosteroids. These are drugs that target different levels of the immune response chain and are not always effective.
Research is advancing rapidly to discover new, more efficient molecules. These are expensive drugs that are not always available.
Radiotherapy
Can be very helpful in the management of OD. It potentiates the effect of corticosteroids and improves ocular motility and diplopia.
Eyelid surgery
OD can cause eyelid retraction and the eyes become wide open. Some patients may have difficulty closing their eyelids, this can make the eyes and cornea more exposed which causes excessive dryness and eye discomfort.
Surgical repositioning of the eyelids is usually done after 3 months of stability and hormonal balance, this allows a reduction in functional signs and an improvement in the aesthetic appearance of the patient.
Eye muscle surgery
In OD, the muscles may be affected by the disease, become inflamed with edema and increased volume, this varies from muscle to muscle. As the disease stabilizes, muscle fibrosis sets in in favor of a scarred appearance. This can affect motility and especially the synchronization of movements of both eyes. You may have diplopia (double vision) or strabismus.
Faced with constant diplopia, a prism can improve the gene. In front of a strabismus that has not progressed (at a scarring stage) muscle surgery is required.
Orbital decompression surgery
It consists of increasing the orbital volume by removing the walls that limit the orbit with the sinuses around. You can remove the inner wall, the bottom wall (floor of the orbit) and the outer wall. Dr Ben said performs decompression using hidden incisions that cannot be seen.
This surgery can only be performed if the disease is completely stable with a balanced thyroid workup for the past 3 months. It is done first before muscle and eyelid surgery.
This surgery, which increases the size of the orbit, may be combined with excision of the periocular fat, thus giving the eye more space to move back.
Decompression is indicated in the majority of cases for aesthetic purposes to recover the gaze and improve clinical symptoms. In rare cases and in the face of compression of the optic nerve with a risk of loss of visual acuity which is due to a posterior volumetric increase in the muscles, decompression must be done urgently to free the optic nerve and avoid loss of 'AV ..